News & Events
News & Events
News
May 22, 2017
Cell therapies for diabetes benefit from anti-allergy drugs
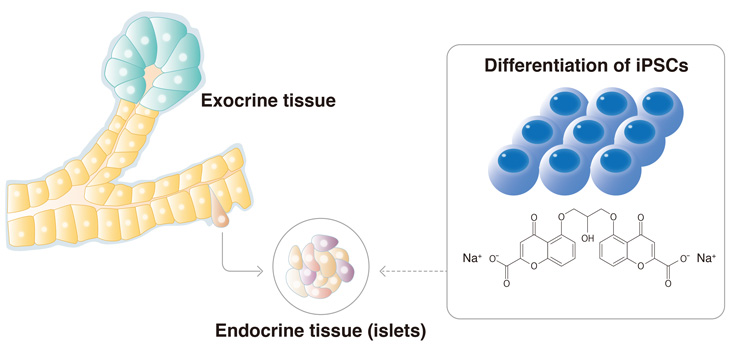
The addition of sodium cromoglicate improves the differentiation of iPSCs to pancreatic cells.
could differentiate iPS cells to islets cells.
Despite its high frequency, type I diabetes, in which the body's immune system destroys the cells responsible for producing insulin, can actually be treated effectively with the transplantation of islet cells or whole organ pancreas. The problem is that there are few donors for these transplants, which has led scientists to prepare cell transplants in the lab. In its latest study, the Professor Kenji Osafune lab has found that the drug compound sodium cromoglicate is effective at inducing iPS cells into islet cells for potential patient care.
"Transplantation therapy is limited by donor shortage and tissue rejection. Differentiating iPS cells into islet cells could solve this problem," he said.
The ability to prepare human islet cells from iPS cells already exists, but the costs and time make them clinically impractical.
"Small molecule inducers are preferred to differentiate iPS cells because they are cheap," noted Osafune.
His lab conducted a drug screening on over a thousand compounds, finding sodium cromoglicate as a molecule that promotes iPS cell differentiation to endocrine. Sodium cromoglicate is not unknown in the medical world, as it is commonly used in anti-allergy drugs.
Osafune was not surprised that a substance affecting the immune system could also play a role in islet cell production. "Many compounds affect many systems in the body. It is why as a doctor I always have to consider side effects."
The pancreas can be divided into two sections. The exocrine pancreas is responsible for food digestion, while the endocrine pancreas is responsible for insulin secretion, and mixing the two in cell transplantations could compromise the treatment. Osafune found that sodium cromoglicate biased the differentiation of iPS cells to endocrine pancreas, suggesting the protocol minimized the risk of contaminating cells.
"Clinical therapies depend not only on a large cell population, but also a homogeneous population," he said.
At the moment, the number of islet cells produced by sodium cromoglicate is modest compared to methods too expensive for clinical application. However, using sodium cromoglicate, Osafune could identify specific molecular pathways that may enhance the differentiation of iPS cells to islet cells. New compounds that target this signaling could produce more islet cells in the lab.
"We found that sodium cromoglicate depresses BMP signaling. Modulating this signaling may increase the number of islet cells," he said.
Paper Details
- Journal: Diabetologia
- Title: Identification of a small molecule that facilitates the differentiation of human iPSCs/ESCs and mouse embryonic pancreatic explants into pancreatic endocrine cells
- Authors: Kondo Y1,2, Toyoda T1, Ito R1,2, Funato M1, Hosokawa Y1, Matsui S1, Sudo T1, Nakamura M1, Okada C1,3, Zhuang X2, Watanabe A1, Ohta A1, Inagaki N2 and Osafune K1
- Author Affiliations:
- Center for iPS Cell Research and Application (CiRA), Kyoto University, Kyoto, Japan
- Department of Diabetes, Endocrinology and Nutrition, Kyoto University, Kyoto, Japan
- Mitsubishi Space Software, Amagasaki, Japan