
Research Activities
Research Activities
Publications
August 09, 2017
Physical force benefits diabetes therapy
The addition of chemical inhibitors simplifies the culture method used to generate pancreatic progenitor cells from iPSCs.
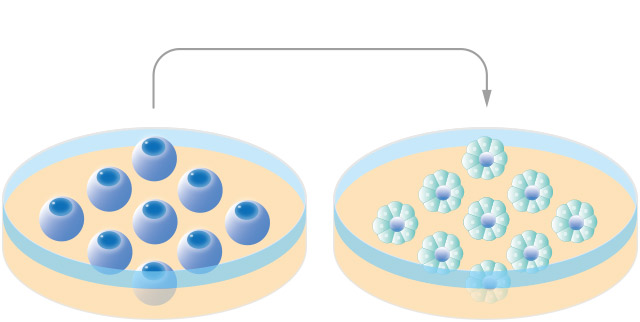
Cell therapies that involve the transplantation of insulin-secreting cells have shown promising success for diabetes treatment. To produce insulin-secreting cells, iPS cells are differentiated into pancreatic progenitor cells through culturing. Two types of culture systems, cell aggregation (3D) and monolayer (2D) culture systems, are used, but vary significantly in the number of pancreatic progenitor cells produced. In a project led by Junior Associate Professor Taro Toyoda, the Kenji Osafune lab at CiRA has found the different efficiencies of the two systems can be attributed to the biomechanics of the cell. They further show that controlling the expression of proteins responsible for the biomechanics enhances the production of pancreatic progenitor cells.
Scientists have had much more success generating pancreatic progenitor cells in aggregation culture systems, but monolayer culture systems offer an easier and stable way to produce the cells.
"Aggregation cultures cause mechanical stress on cells that does not exist in monolayer cultures. We looked for cytoskeletal proteins that are differentially regulated in the two conditions," said Toyoda.
Cytoskeleton proteins determine the biomechanics of a cell. For an iPS cell to differentiate into a pancreatic progenitor cell, a number of morphological changes must occur. These changes depend on the cytoskeleton protein myosin II.
By comparing pancreatic progenitor cells made in the two cultures, Toyoda found that the suppression of non-muscle myosin II is key for the successful differentiation of iPS cells. Therefore, to enhance the pancreatic progenitor cell production in monolayer culture, he added a myosin II inhibitor to the system.
"We added to standard protocols for pancreatic progenitor cells myosin II inhibitors and ROCK inhibitors," he said.
ROCK molecules are known to affect many cellular mechanisms including the cytoskeleton, and they too were suppressed in cells in aggregation culture. Mixing ROCK and non-muscle myosin II inhibitors into monolayer culture, Toyoda found, induced the differentiation of human iPS cells into pancreatic progenitor cells in a manner consistent with aggregation culture.
The resulting human pancreatic progenitor cells were then injected into mice. Thereafter, the mice began to secrete human insulin, suggesting the implanted progenitor cells went on to transform into insulin-producing cells.
While scientists have had greater success producing pancreatic progenitor cells in aggregation culture, it is hard to standardize the culture system because inhibitors reach only cells on the surface in aggregation culture. On the other hand, they reach all cells in monolayer culture.
"Cell therapies for diabetes are effective. Our goal is to simplify protocols that differentiate iPS cells into insulin-producing cells to take these therapies to the clinic faster," said Osafune.
Paper Details
- Journal: Stem Cell Reports
- Title: Rho-Associated Kinases and Non-muscle Myosin IIs Inhibit the Differentiation of Human iPSCs to Pancreatic Endoderm
- Authors: Toyoda T, Kimura A, Tanaka H, Ameku T, Mima A, Hirose Y, Nakamura M, Watanabe A, and Osafune K
- Author Affiliations:
Center for iPS Cell Research and Application (CiRA), Kyoto University, Kyoto, Japan






















