
News & Events
News & Events
News
April 04, 2017
Engineering heart cells
CiRA researchers show that survival of grafted cells
depends on the geometry of the graft.
the geometry of a graft influences heart transplantation outcomes.
Scientists from CiRA and the University of Louisville in the United States report the effective therapeutic function of engineered cardiac tissue (ECT) made from human iPS cells for heart failure. ECT were made on custom polymer molds so that cellular components and geometry could be modified. Certain geometries were consistent with better cell survival and function following the transplantation of ECT into animal hearts.
Patients suffering from heart failure struggle to recover because their hearts cannot replace lost heart muscle cells. The transplantation of ECT made from stem cells has shown good promise to regenerate the lost cells, but the clinical use of ECT remains in the future.
"ECT transplants work excellently in rats. Generating large enough ECTs that function in humans is next step," said CiRA Professor Jun Yamashita.
Two major problems lie in the clinical application of ECT. First is the production of enough heart cells and second is shaping the ECT to maximize cell function. The first problem can be solved with iPS cells, of which Yamashita is an expert, and the second can be solved with bioengineering, which is why Professor Bradley B. Keller of Louisville joined the project.
"My lab and Jun's lab have been working together many years on innovative iPS heart therapies," said Keller.
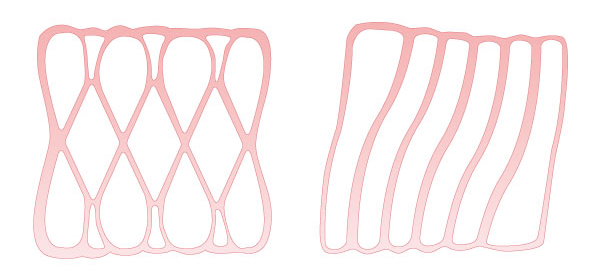
To identify the best conditions for ECT fabrication, tissue molds of the same size but of different patterns were loaded with different number of cells. The ECT were then transplanted into the damaged hearts of rats, Unexpectedly, the transplantation of ECT loaded with fewer cells resulted in better structural and functional heart recovery.
Yamashita said that different geometries of the ECT could explain why fewer cells were more effective.
"Asymmetrically shaped ECTs could vary the mechanical stress or nutrition supply to the cells," he said.
Furthermore, loading the mold with more cells could cause competition for oxygen, which would lead to suboptimal performance.
Another factor that has limited ECT prepared from stem cells is the maturation of the resulting heart cells.
"Normally, heart cells derived from stem cells are of the fetal type," said Yamashita.
Fetal heart cells and adult heart cells show different beating and force generation, which compromises the quality of the recovery following transplantation. The study shows that reducing the asymmetry corresponded with more maturation, but the reasons remain unknown.
"Our ECTs are scalable, so we should be able to make sizes large enough for patients. They also show good structure, function, and maturation. What we do not yet understand are the biological factors responsible for recovery after implantation onto the heart," said Keller.
Paper Details
- Journal: Scientific Reports
- Title: Impact of cell composition and geometry on human induced pluripotent stem cells-derived engineered cardiac tissue
- Authors: Takeichiro Nakane1,2,3, Hidetoshi Masumoto1,2,3, Joseph P Tinney1,4, Fangping Yuan1,4, William J Kowalski1,4, Fei Ye1,4, Amanda J LeBlanc5, Ryuzo Sakata3, Jun K Yamashita2, and Bradley B Keller1,4
- Author Affiliations:
- Kosair Charities Pediatric Heart Research Program, Cardiovascular Innovation Institute, University of Louisville, Louisville, KY, USA
- Center for iPS Cell Research and Application (CiRA), Kyoto University, Kyoto, Japan
- Department of Cardiovascular Surgery, Kyoto University, Kyoto, Japan
- Department of Pediatrics, School of Medicine, University of Louisville, Louisville, KY, USA
- Department of Physiology, University of Louisville, Louisville, KY, USA






















