
News & Events
News & Events
News
November 14, 2024
Enhancing the efficacy of cell transplantation therapy for stroke or traumatic brain injury
Research Overview
When the motor cortex of the brain is damaged due to traumatic brain injury or stroke, it can result in long-term motor paralysis and significant motor function impairment. Although treatments such as drug therapy, surgery, and rehabilitation are commonly employed, their effectiveness is limited due to the low regenerative capacity of the central nervous system (CNS), thus necessitating the development of curative therapies. Cell transplantation therapy using human induced pluripotent stem cell (iPSC)-derived brain organoids has gained attention as a promising new treatment approach to repair damaged neural circuits and promote the recovery of motor functions. However, the success rate remains low due to acute cell death after cell transplantation.
Research Findings
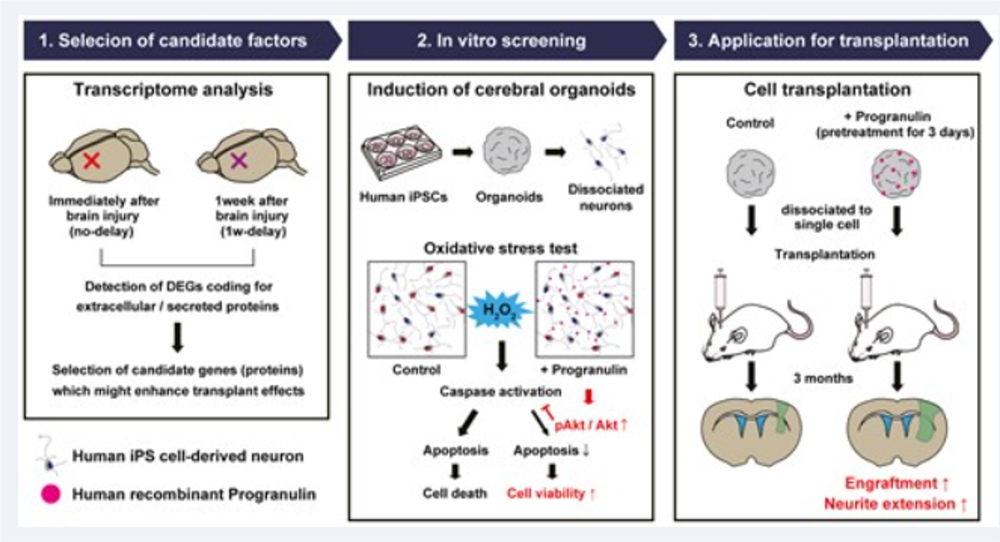
Previous reports have shown that cell transplantations one week after traumatic brain injury lead to better outcomes in terms of cell engraftment and neuronal axonal extension compared to transplants immediately following injury. Based on those observations, the research group hypothesized that brain tissues one week after traumatic brain injury may offer a more favorable environment for cell transplantation than immediately after injury. As such, they sought to identify candidate substances responsible for the more permissive environment at the latter time point. The group found several candidate substances through transcriptome analysis, comparing RNA expression in brain tissues immediately and one week after injury. Cell toxicity tests were performed using neurons derived from brain organoids to evaluate the ability of these candidate substances to protect against oxidative stress, a common cause of neuronal cell death following strokes and traumatic brain injuries. The study found that treatment with progranulin (PGRN), a growth factor, reduced apoptosis through Akt phosphorylation and enhanced neuron survival. Furthermore, to validate the therapeutic effects of PGRN-treated human iPSC-derived brain organoids (hiPSC-COs), the researchers transplanted hiPSC-COs treated with recombinant human PGRN (rhPGRN) into mouse brains and performed histological evaluations three months later. The results showed a significant improvement in the engraftment efficiency of hiPSC-COs, with enhanced axonal extension along the corticospinal tract, in the rhPGRN-treated group compared to the untreated group.
Application of Research Findings
Based on these results, rhPGRN is believed to act as a priming agent to enhance engraftment and axonal extension of iPSC-derived neurons during cell transplantation therapy. Further studies will be necessary to identify optimal administration routes and evaluate safety (e.g., tumor formation) to ensure safer and more effective cell transplantation therapies.
Paper Details
- Journal: Stem Cells Translational Medicine
- Title: Progranulin enhances the engraftment of transplanted human iPS cell-derived cerebral neurons
- Authors:
Keitaro Yamagami1,2, Bumpei Samata1, Daisuke Doi1, Ryosuke Tsuchimochi1,2, Tetsuhiro Kikuchi1, Naoya Amimoto1, Megumi Ikeda1, Koji Yoshimoto2, Jun Takahashi1*
*: Corresponding author - Author Affiliations:
- Department of Clinical Application, Center for iPS Cell Research and Application, Kyoto University
- Department of Neurosurgery, Kyushu University Graduate School of Medical Sciences, Kyushu University






















