
Research Activities
Research Activities
Publications
October 25, 2018
Mutant pancreatic cells will not die
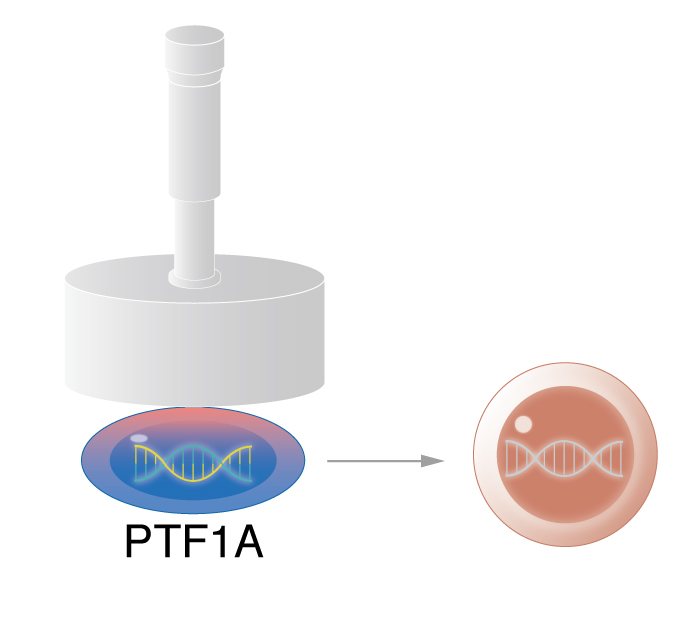
Acinar cells that fail to express PTF1A and under stress, tend to show a different cell identity, suggesting a possible route to becoming cancerous.
Pancreatic cancer is the deadliest of cancers, and there has been hardly any change in survival rates in the past 40 years. In many cases, patients have a mutated cancer gene. However, it is known that cell stress in combination with the mutated cancer gene increases the risk, at least in mice. In a new study in Scientific Reports, CiRA scientists show how the loss of one gene, Ptf1a, in mice triggers cell stress, leading to potentially cancerous changes in the pancreas.
The pancreas is an unusual organ in that can be viewed as two glands mixed into one. The exocrine pancreas secretes enzymes for digestion, while the endocrine pancreas releases hormones like insulin. Although these two functions are distinct, the genes responsible for growing the pancreas must assure both systems operate normally.
During the development of digestive organs, "we know PTF1A is indispensable for pancreatic formation. Cells expressing PTF1A become acinar cells. Those that don't become duodenal or bile duct cells," says CiRA Professor and pancreatic surgeon Yoshiya Kawaguchi, who led the study.
The importance of this gene has been mostly studied during the development of the pancreas. However, PTF1A also exists in adults, well after the pancreas has formed.
"There is evidence that PTF1A is responsible for the secretion of digestive enzymes from the pancreas. More importantly, there is evidence that its loss is related to pancreatic cancer, but the precise mechanism was unrevealed," continues Kawaguchi.
These observations have mostly come from heterozygous mice, that is, mice in which one of the two Ptf1a alleles is knocked out. A mouse in which the gene is knocked out of both alleles would have valuable new information about PTF1A function in adult cells.
"A homozygous mutant allows us to investigate more extreme effects of PTF1A," says Dr. Morito Sakikubo, the first author of the study and also a pancreatic surgeon.
Unsurprisingly, the loss of PTF1A resulted in these mice having smaller pancreas due to apoptosis, or programmed cell death.
"We viewed the cells with electron microscopy and found the cells underwent endoplasmic reticulum stress," says Sakikubo. Endoplasmic reticulum stress is often the result of unfolded or misfolded proteins, and apoptosis is a common response by any cell, not just acinar cells.
Unfolded and misfolded proteins trigger an unfolded protein response that involves the molecules ATF4 and ATF6. These molecules correct the folded protein to relieve the cell of endoplasmic reticulum stress, but if active too long, they indicate to the cell that the stress is too great to overcome, and the cell activates CHOP, a molecule that signals apoptosis.
Many stressed cells, though, can escape apoptosis by changing their identity, a process known as metaplasia. These cells risk becoming cancerous.
Kawaguchi notes that the defective apoptosis seen in the homozygous mouse mutants could clarify the relationship between PTF1A and pancreatic cancer.
"Apoptosis is a healthy process through which the body kills off stressed cells. Cells that escape apoptosis can become cancerous upon the oncogenic gene mutations. Understanding the molecular pathways responsible should lead to better prevention and treatments," he says.
Paper Details
- Journal: Scientific Reports
- Title: Ptf1a inactivation in adult pancreatic acinar cells causes apoptosis through activation of the endoplasmic reticulum stress pathway
- Authors: Morito Sakikubo1,2, Kenichiro Furuyama1,2, Masashi Horiguchi1,2, Shinichi Hosokawa1,2, Yoshiki Aoyama1,2, Kunihiko Tsuboi1,2, Toshihiko Goto1,2, Koji Hirata1,2, Toshihiko Masui1,2, Yuval Dor3, Tomoyuki Fujiyama4,5, Mikio Hoshino4, Shinji Uemoto1 and Yoshiya Kawaguchi2
- Author Affiliations:
- Department of Hepato-Biliary-Pancreatic Surgery and Transplantation, Kyoto University Graduate School of Medicine, Kyoto, Japan
- Center for iPS cell Research and Application, Kyoto, Japan
- Department of Developmental Biology and Cancer Research, The Institute for Medical Research Israel-Canada, Hebrew University-Hadassah Medical School, Jerusalem, Israel
- Department of Biochemistry and Cellular Biology, National Institute of Neuroscience, NCNP, Tokyo, Japan
- International Institute for Integrative Sleep Medicine (WPI-IIIS), University of Tsukuba, Tsukuba, Japan






















